Hand touching brain and network connection on glitter bright lights colorful background
THE BRAIN: STRUCTURE, FUNCTION, AND IMPAIRMENT
Structure and Function
The brain consists of two hemispheres. The left hemisphere controls the right side of the body and is thought to be more involved in language functions, logical inference, and detail analysis in almost all right-handed individuals and a good many lefthanders as well. The right hemisphere controls the left side of the body. It is more involved in visual-spatial skills, creativity, musical activities, and the perception of direction. But again, note that some lefthanders may reverse this hemispheric pattern. The two hemispheres communicate with one another via the corpus callosum, which helps to coordinate and integrate our complex behavior. Each cerebral hemisphere has four lobes: the frontal, temporal, parietal, and occipital lobes (see Figure).
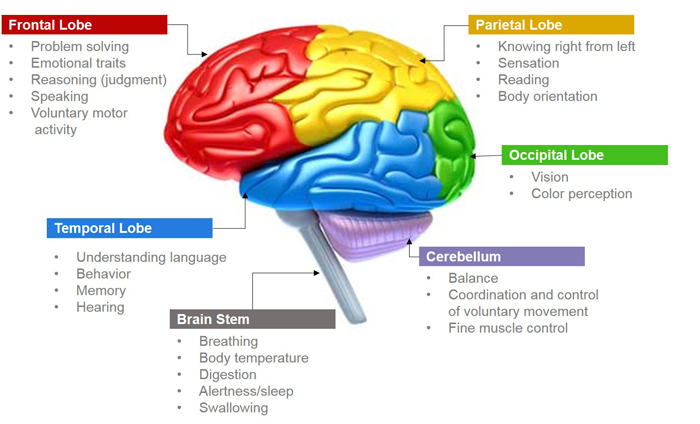
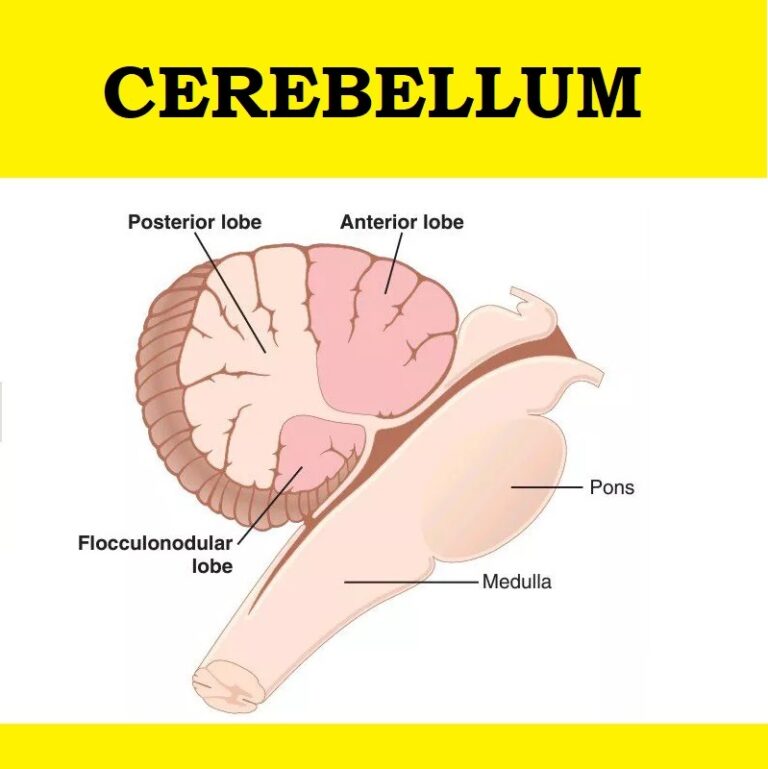
The frontal lobes are the most recently developed parts of the brain, from both an evolutionary and developmental perspective. They enable us to observe and compare our behavior and the reactions of others to it in order to obtain the feedback necessary to alter our behavior to achieve valued goals. Also associated with the frontal lobes are executive functions— formulating, planning, and carrying out goal-directed initiatives. Finally, emotional modulation—the ability to monitor and control one’s emotional state—is also associated with frontal lobe functioning. Substantial frontal lobe development occurs in adolescence. The temporal lobes mediate linguistic expression, reception, and analysis. They are also involved in auditory processing of tones, sounds, rhythms, and meanings that are nonlanguage in nature. The parietal lobes are related to tactile and kinesthetic perception, understanding, spatial perception, and some language understanding and processing. They are also involved in body awareness. The occipital lobes are mainly oriented toward visual processing and some aspects of visually mediated memory. Motor coordination, as well as the control of equilibrium and muscle tone, is associated with the cerebellum.
Antecedents or Causes of Brain Damage
What causes brain damage? There are a number of possibilities.
Trauma: It is estimated that brain injury occurs in more than 500,000 Americans every year (Zillmer et al., 2008). Incidents producing these injuries range from automobile accidents, to sports injuries, to falls off a stepladder. The outcomes are wideranging, and the nature of the head injury (e.g., closed vs. open/penetrating) may have implications as well. Although most head injuries are considered mild, a substantial percentage of cases require hospitalization. Head trauma is a leading cause of death and disability in young Americans (Zillmer et al., 2008). The major effects of head trauma can be categorized as concussions, contusions, and lacerations. Concussions (jarring of the brain) usually result in momentary disruptions of brain function, although permanent damage is uncommon (unless there are repeated concussions, as might be the case in football, soccer, or boxing, for example). Contusions refer to cases in which the brain has been shifted from its normal position and pressed against the skull. As a result, brain tissue is bruised. Outcomes can often be severe and may be followed by comas and deliriums. Lacerations involve actual ruptures and destruction of brain tissue. They can be caused by bullets or flying objects, for example. These lacerations are, of course, exceedingly serious forms of damage.
Cerebrovascular Accidents: The blockage or rupture of cerebral blood vessels is often termed a “stroke.” This is a very common cause of brain damage in adults, and stroke is one of the leading causes of death in the United States (and other countries). Although primarily occurring in the elderly, stroke is also one of the most common causes of death in middle-aged adults. In occlusions, a blood clot blocks the vessel that feeds a particular area of the brain. This can result in aphasia (language impairment), apraxia (inability to perform certain voluntary movements), or agnosia (disturbed sensory perception). In the case of a cerebral hemorrhage, the blood vessel ruptures and the blood escapes onto brain tissue and either damages or destroys it. The exact symptoms that ensue depend on the site of the accident and its severity. In very severe cases, death is the outcome. Those who survive often show paralysis, speech problems, memory and judgment difficulties, and so on. It is very important to get stroke patients to the hospital immediately. Medications that essentially dissolve occlusions (“clot-busting” medications) can limit the permanent damage from occlusive strokes. In addition, new medications are being developed that prevent the cascade of chemical reactions responsible for neuronal damage or even death (e.g., tissue plasminogen activator, tPA). Therefore, in many cases, prompt action can be of major benefit.
Tumors: Brain tumors may grow outside the brain, within the brain, or result from metastatic cells spread by body fluids from some other organ of the body, such as the lung or the breast. Initial signs of brain tumors are often quite subtle and can include headaches, vision problems, gradually developing problems in judgment, and so on. As the tumor grows, so does the variety of other symptoms (e.g., poor memory, affect problems, or motor coordination). Tumors can be removed surgically, but the surgery itself can result in more brain damage. Some tumors are inoperable or located in areas too dangerous to operate on. In such cases, radiation treatments are often used.
Degenerative Disease: This group of disorders is characterized by a degeneration of neurons in the central nervous system. Common degenerative diseases include Huntington’s chorea, Parkinson’s disease, and Alzheimer’s disease and other dementia. Alzheimer’s disease is the most common degenerative disease (age of onset is typically 65 years old or older), followed by Parkinson’s disease (age of onset 50 to 60 years old), and finally, Huntington’s chorea (age of onset 30 to 50 years old). In all three cases, there is progressive cerebral degeneration along with other symptoms in the motor areas. Eventually, patients in these categories show severe disturbances in many behavioral areas, including motor, speech, language, memory, and judgment difficulties. More and more, neuropsychologists are attempting to identify and diagnose early stages of diseases like Alzheimer’s in order to provide treatment that may have maximal impact on future functioning (Bondi, Jak, Delano-Wood, Jacobson, Delis, & Salmon, 2008).
Nutritional Deficiencies: Malnutrition can ultimately produce neurological and psychological disorders. They are most often observed in cases of Korsakoff’s psychosis (resulting from nutritional problems brought about by poor eating habits common in longtime alcoholics), pellagra (niacin/vitamin B3 deficiency), and beriberi (thiamin/vitamin B1 deficiency).
Toxic Disorders: A variety of metals, toxins, gases, and even plants can be absorbed through the skin. In some instances, the result is a toxic or poisonous effect that produces brain damage. A very common symptom associated with these disorders is delirium (disruption of consciousness).
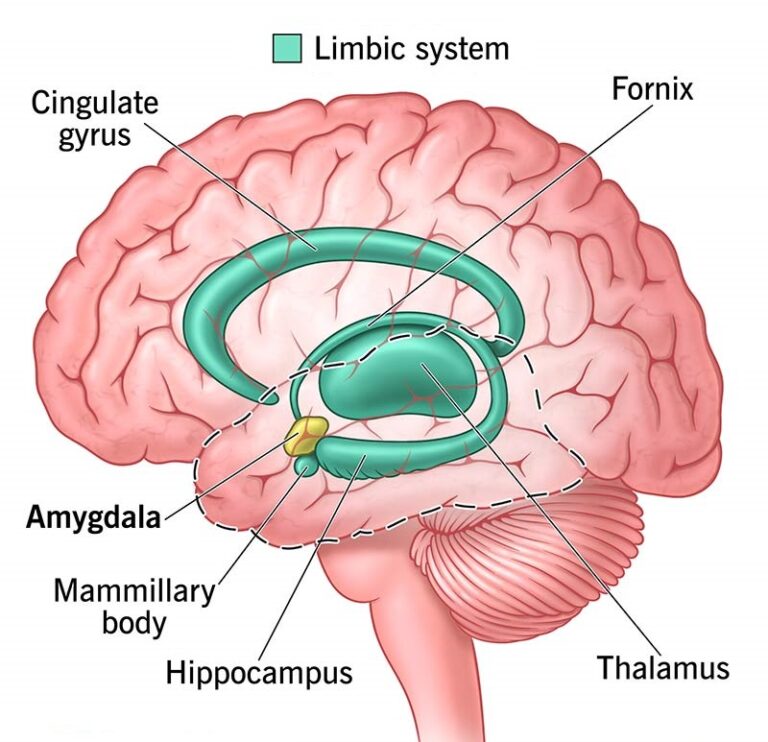
Chronic Alcohol Abuse: Chronic exposure to alcohol often results in tolerance for and dependence on the substance. Tolerance and dependence appear to have neurological correlates, including, for example, changes in neurotransmitter sensitivity and shrinkage in brain tissue. Several regions of the brain seem especially vulnerable to damage from chronic exposure to alcohol (Oscar-Berman & Marinkovic, 2003, 2007; U.S. Department of Health and Human Services, 2000). We highlight only a few of the most consistent findings here. The limbic system is a network of structures within the brain associated with memory formation, emotional regulation, and sensory integration. Studies of alcoholics have indicated deficits in these areas of functioning. The diencephalon is a region near the center of the brain that includes the mammillary bodies of the hypothalamus. Studies suggest shrinkage or lesions in these areas as a result of chronic alcohol exposure, and memory deficits in alcoholics are consistent with these findings. Several studies have also reported findings that suggest alcoholics evidence atrophy of the cerebral cortex. Finally, damage to the cerebellum, responsible for motor coordination, is also well documented. A history of accidental falls or automobile accidents may suggest neurological damage resulting from alcohol abuse/dependence.
Consequences and Symptoms of Neurological Damage: Brain injury or trauma can produce a variety of cognitive and behavioral symptoms. Unfortunately for the diagnostician, many of these symptoms may also occur in connection with traditional mental disorders. Moreover, patients’ responses to neurological impairment may give rise to psychological and emotional reactions. For example, an individual with neurological damage may become depressed over the inability to manage certain daily tasks. This in turn can easily obscure the process of differential diagnosis. These difficulties aside, several common symptoms associated with neurological damage are in the list that follows. However, each of these may occur in every disorder, and there is considerable variation among patients with the same disorder.
1. Impaired orientation: inability, for example, to say who one is, name the day of the week, or know about one’s surroundings.
2. Impaired memory: patient forgets events, especially recent ones, sometimes confabulates or invents memories to fill the gaps, and may show impaired ability to learn and retain new information.
3. Impaired intellectual functions: comprehension, speech production, calculation, and general knowledge may be affected (e.g., cannot define simple words, name the U.S. president, or add figures).
4. Impaired judgment: patient has trouble with decisions (e.g., cannot decide about lunch, when to go to bed, etc.).
5. Shallow and labile affect: person laughs or weeps too easily and often inappropriately; shifts from joy to tears to anger, for example, very rapidly.
6. Loss of emotional and mental resilience: patient may function reasonably well under normal circumstances, but stress (e.g., fatigue, mental demands, emotional upset) may result in deterioration of judgment, emotional reactions, and similar problems.
7. Frontal lobe syndrome: a group of personality characteristics often follow the destruction of frontal lobe tissue through surgery, tumor, or injury. Typical symptoms are impaired impulse control, poor social judgment and planning ability, lack of concern over the consequences of one’s actions, apathy and indifference, some suspiciousness, and temper tantrums.